What’s more likely to kill Americans—gun violence, car accidents or opioid overdoses?
Today, it’s opioids, according to a recently released report by the National Safety Council.
But how can a prescribed painkiller lead to death? Surprisingly, opioids become addictive more quickly than most people think they can. A little knowledge about opioids and alternative treatments can help keep people safe and best manage their pain.
What are opioids?
- Prescribed pain management drugs
- Intended to help with cancer-related or post-surgical pain
- Highly addictive and not intended to address chronic pain
- Recommended for no more than three days use for non-cancer, non-surgical pain (by the Centers for Disease Control (CDC), Food and Drug Administration (FDA) and National Academy of Medicine (NAM)
The opioid epidemic has exploded in the last 20 years, since doctors began prescribing these drugs more frequently for pain management. At the time, pharmaceutical companies advertised that opioids were nonaddictive and highly effective for pain. Statistics from the past several decades tell a different story.
What are the risks?
Opioid addiction happens quickly and easily. Tolerance to the drug and dependence on it usually catches people by surprise.
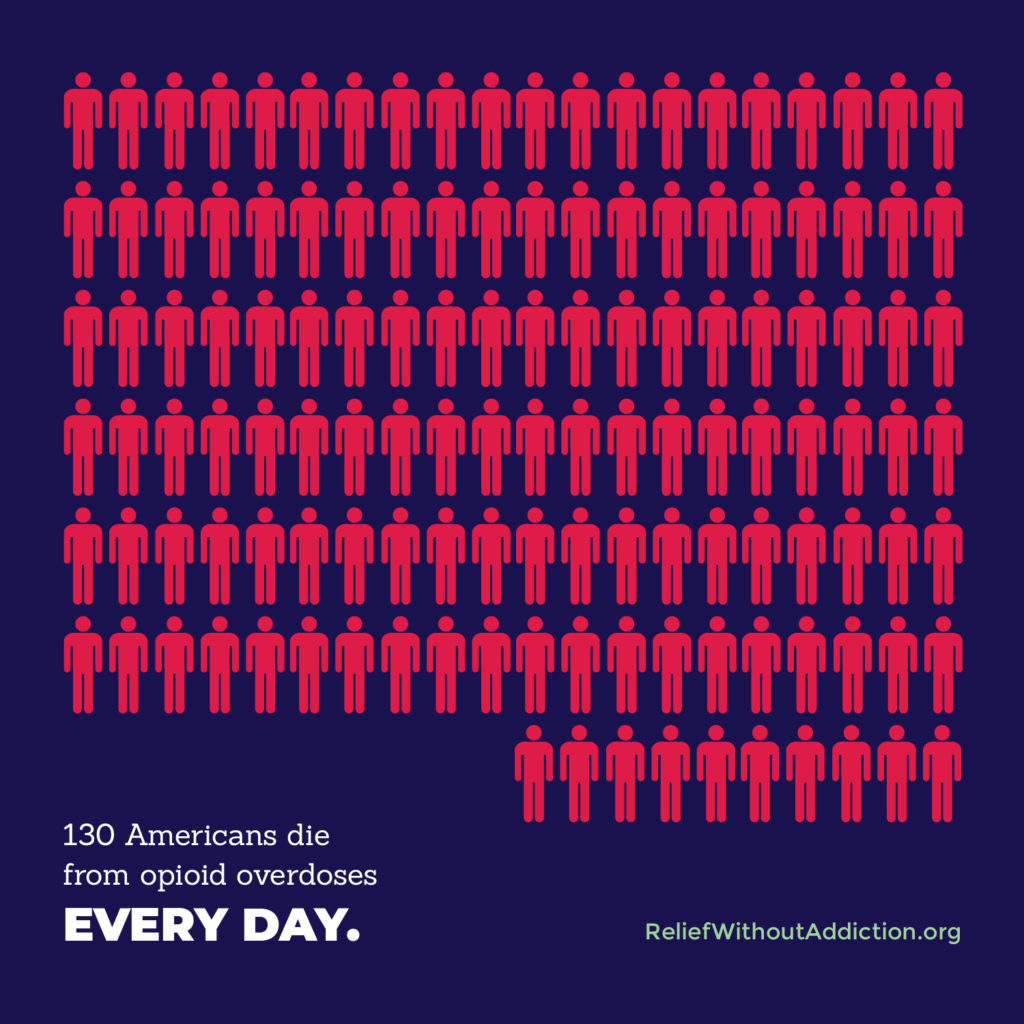
Addiction and accidental death from opioid overdose can happen to anyone. It does not discriminate by age, sex or income level. All communities with people who suffer from chronic pain are vulnerable.
- 130 Americans die from opioid overdoses every day (US Department of Health and Human Services).
- Opioid overdose deaths have quadrupled since 1999 (CDC).
- Americans consume up to 80% of the world’s prescription opioids (CDC).
- Opioid abuse is now responsible for more deaths than from all illicit drug use combined.
- Fueled by drug-related offenses, the United States now incarcerates a greater number of people and a greater percentage of its population than any other country.
Is there an alternative? Yes!
The CDC, FDA and NAM all recommend care without drugs as the first response for pain relief. Common examples include:
- Chiropractic care
- Heat, massage or acupuncture
- Behavioral modification strategies
If a doctor recommends opioids for chronic pain, explore some of these options first. If a specific medical situation calls for the use of a prescription opioid, every dose should be evaluated. Does the patient need this drug right now? What else can be done to alleviate the pain?
How chiropractic care can help
Chiropractic care provides a drug-free alternative with natural pain relief. Through spinal adjustments and soft tissue care, chiropractors can ease general and lower back pain and the physical symptoms that cause its recurrence.
Chiropractic treatment is cost-effective and available everywhere. Most offices see patients quickly for personalized and non-invasive care. Most times, patients don’t need a referral.
Like medical doctors, chiropractors are highly trained. They are licensed and regulated. With a caring and hands-on approach, chiropractors are eager to help each patient best manage their unique pain.
Chiropractic therapy does not mask back pain. Instead, it aims to restore movement and function by addressing what causes the pain.